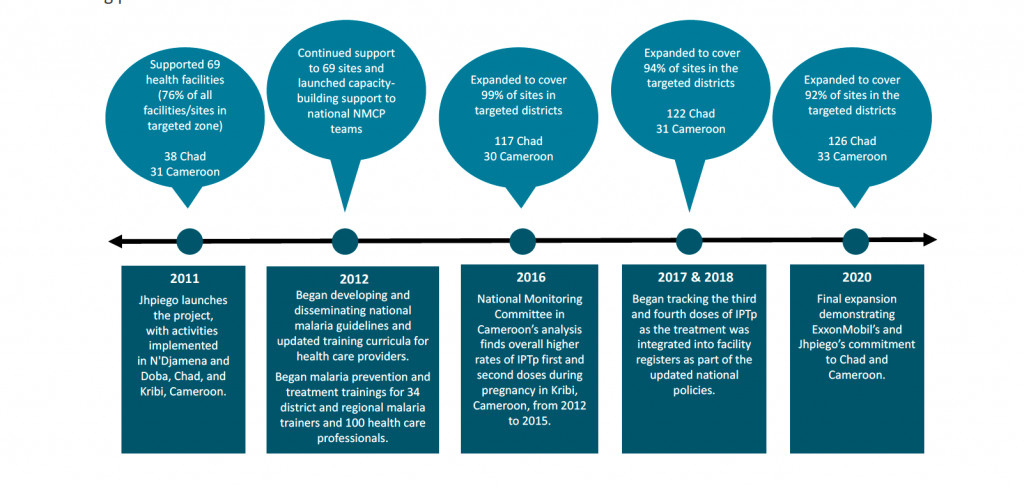
ExxonMobil Foundation’s 10-year partnership with Jhpiego in Chad and Cameroon began as an inspired effort to prevent malaria in pregnant women in three small districts along the petroleum pipeline. Over the decade, the initial project grew in scope and success. Health workers in key areas improved their skills to prevent and treat malaria, community education and outreach expanded, and more than 1.3 million women and families benefited from the strategic interventions.
Jhpiego’s technical expertise and experience, supported by the Foundation’s dedicated funding, led to stronger national prevention and treatment policies and strategies, improved service delivery and engaged communities in sustaining their progress. The national prevention and treatment policies further led Jhpiego to focus on increasing the rate of pregnant women receiving preventive malaria medicine.
Malaria is a deadly threat to pregnant women and their babies, responsible for many severe maternal illnesses and death and up to 200,000 newborn deaths a year. The delivery of high quality antenatal care (ANC) is essential for successful malaria in pregnancy (MiP) programming. The World Health Organization (WHO) Recommendations on Antenatal Care for a Positive Pregnancy Experience promote increased support of women during their pregnancies with comprehensive care, including MiP interventions. By integrating malaria prevention/treatment during ANC, health systems improve maternal and newborn outcomes by combating maternal anemia, stillbirth, prematurity and low birthweight.
Preventing Malaria in Pregnancy

Within a year of the partnership’s inception, the percentage of pregnant women in Chad who received their first dose of preventive malaria medicine increased more than fivefold, from 12% in the first quarter of 2012 to 63% in the fourth quarter; and the percentage who received the second dose more than doubled, from 14% to 36%. From 2013 to 2015, Jhpiego provided technical guidance to the countries’ National Malaria Control Programs and led the development of national-level manuals and guidelines on the prevention and treatment of malaria in communities through home-based interventions, integrated supervision and intermittent preventive treatment (IPT) for pregnant women.
In October 2016, the National Monitoring Committee in Cameroon released an evaluation of the project, including a comparative analysis of key project indicators in Kribi district versus all other districts in the Sud Region. The analysis revealed higher rates of IPT during pregnancy (first and second doses) in the Kribi district, a direct result of the technical guidance at the national level.
In 2018, Jhpiego began tracking the third and fourth doses of IPT (IPTp3 and IPTp4) as the treatment was integrated into the health facility registers as part of the updated national policies. In Chad, the rate improved from 26.1% at baseline to 36% (IPTp3) and from 7.5% to 17% (IPTp4). In Cameroon, the rate improved from 39% at baseline to 47% (IPTp3) and from 18% to 22% (IPTp4).
Prompt Testing and Appropriate Treatment of Malaria
From 2012 to 2020, the project saw a significant improvement in provider capacity to diagnose and treat malaria, with the percentage of cases treated as recommended by national guidelines. Community education played a key role: 118 community health volunteers in Chad and Cameroon have conducted more than a half a million educational sessions, reaching over 654,646 people.
Their work helped deliver results: Since the project’s inception, the cases appropriately treated in Chad steadily increased from 63% to 74% in June 2020. In Cameroon, the cases appropriately treated vastly increased, from 70% in 2012 to 97% in June 2020.
In 2019 in Chad, the percentage of uncomplicated malaria cases confirmed and treated with artemisinin-based combination therapy (ACT) in accordance with national guidelines in health facilities increased from 70% to 94% in 2019, which is higher than the national rate of 91% in 2018. In addition, the percentage of children who were tested using rapid diagnostic tests and treated with ACTs in compliance with national guidelines increased from 68% to 92%.
In Cameroon, the rate of malaria deaths recorded at the Kribi District Hospital decreased from 23% in 2013 to 16% by the end of 2019, which is lower than the national rate of 19% in 2019. However, the overall downward trend has been interrupted by sharp increases every few years. To address this problem, the project engaged managers at the Kribi District Hospital and heads of the health facilities to discuss the importance of timely referral of cases to avoid unnecessary malaria-related deaths. The decrease in malaria-related deaths by the end of 2019 by 10 percentage points (16%) suggests the success of targeting district hospital managers and improvements in timely referral. The foundational experience of this project is wide and deep: 481 health care providers (172 in Chad and 309 in Cameroon) from 159 health facilities have received training in the prevention and management of malaria, data collection and key commodity/stock management and malaria during pregnancy.
The ExxonMobil Foundation-Jhpiego partnership, grounded in experience and expertise, has the potential to raise both countries’ standings in the global malaria rankings. Together, we can deliver on the promise that where a woman lives should not determine if she—or her family—lives.



