When Beatha Mukabucyana’s children fell sick with malaria, a community health worker in her village in Rwanda treated them. “The quick and efficient health services, provided to me in time of need, motivated me to become a community health worker,” she said.
Chosen to serve as a community health worker (CHW) by her village, Karambi, in Nyamasheke District, Beatha now works on the frontlines of PMI Impact Malaria’s efforts to defeat one of the leading causes of death and illness in Rwanda—malaria. This infectious disease, spread by mosquitos, is a major public health concern and priority for the government; in Rwanda, the entire population of 12.9 million people is at risk for malaria. Beatha’s district borders Lake Kivu in western Rwanda and has some of the country’s highest incidence of the deadly disease.

In 2020, Beatha participated in an PMI Impact Malaria-supported training program on integrated community case management (iCCM), which covered malaria and pneumonia and diarrhea for children under five years and home-based management of malaria for children older than five and adults. “The [four day] training was not only an opportunity for me to learn, but also to get answers to all the questions that I encounter while carrying out the duties of a community health worker,” she said.
Now, she handles as many as 20 cases of suspected malaria per month, four to 10 of which are positive cases.
I used to be disheartened seeing sick children and their parents walking long distances to seek care while I was elected to provide the services. At such times, I felt helpless.”
Beatha Mukabucyana
Now, this dedicated CHW can test people with suspected malaria in their own village. She treats those who test positive and, after providing them with the recommended treatment, follows up with them in a few days; she refers people with symptoms of severe malaria to the health facility. She can treat people for test negative for malaria if they have symptoms of diarrhea or pneumonia or refer them to the nearest health facility, if needed.
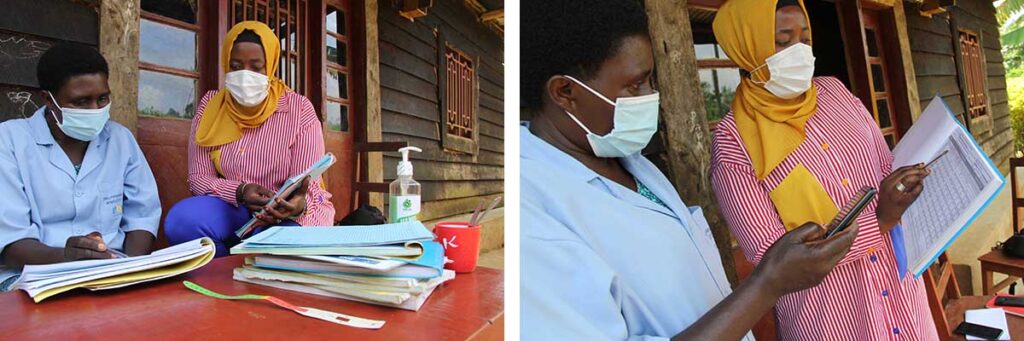
Beatha receives supportive supervision and mentorship from Community Environment and Health Officer Salima Mukeshimana, who works with the 188 CHWs in the 47 villages under the Kamonyi Health Center. Salima mentors the CHWs to educate people about prevention of malaria and other diseases. “I meet the community health workers individually or in small groups at least twice quarterly” she said.
The head of Kamonyi Health Center, Athanase Ntihinyurwa, acknowledges that CHWs have helped reduce the number of malaria cases handled by the health center, which is often overwhelmed by people seeking services. Athanase reported that from January to December 2021, the health center treated 97 positive cases of malaria while CHWs treated 972; many of these people would have had to travel to the health center if help had not been available in their community.
In 2021, in PMI Impact Malaria’s two iCCM supported districts in Rwanda, Nyamasheke and Rusizi, providers at health centers treated 20,651 people and CHWs treated 103,768 people. During that time, 80% of malaria cases were treated in the community in the iCCM supported districts compared to 56% at national level.
Since 2019, PMI Impact Malaria has been working with the national malaria control program in Rwanda to increase quality and access to malaria case management—early diagnosis and prompt and effective treatment—at the community and public facility levels in Nyamasheke and in Rusizi district, just to the south.
PMI Impact Malaria’s iCCM and home-based management of malaria programs have brought care to the community, relieving the pressure on over-burdened health centers and saving lives by saving time.
PMI Impact Malaria is funded and technically assisted by the U.S. President’s Malaria Initiative (PMI) and is led by Population Services International (PSI) in partnership with Jhpiego, Medical Care Development International (MCDI), and the Malaria Elimination Institute (MEI) at UCSF.



